

Investigators also found lower all-cause mortality with intensive targets (1.1% per year vs.
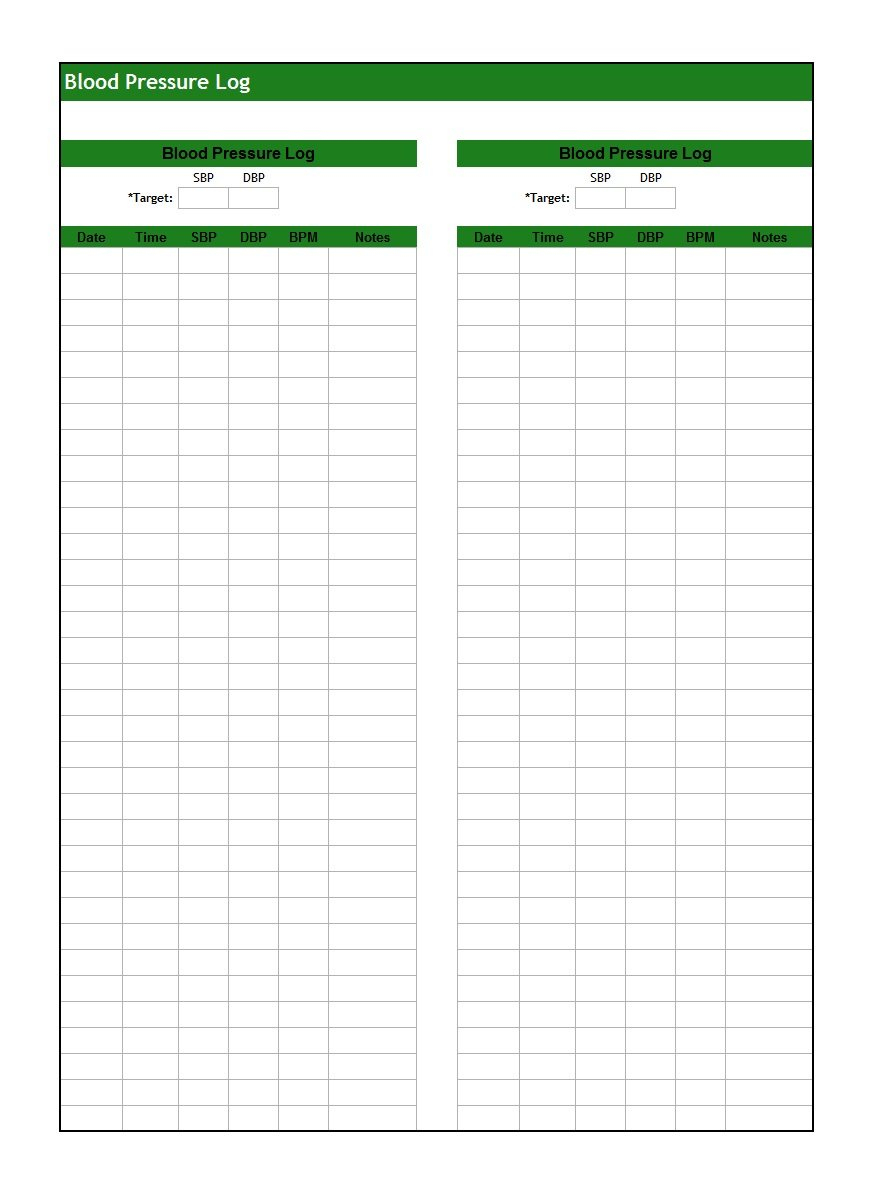
2.4% per year hazard ratio 0.73 95% confidence interval, 0.63 to 0.86). 3,4Īt 3.3 years of follow-up, they found that the lower SBP target resulted in a significantly lower rate of the composite outcome of myocardial infarction, acute coronary syndrome, stroke, acute decompensated heart failure, or cardiovascular death (1.8% per year vs. The Systolic Blood Pressure Intervention Trial ( SPRINT) first published in 2015 (with follow-data published in 2021) randomized 9361 patients with HTN and elevated cardiovascular risk to either an intensive systolic blood pressure (SBP) target (<120 mm Hg) or a standard SBP target (<140 mm Hg). This change was prompted by a growing body of evidence showing a linear relationship between blood pressure and cardiovascular risk, namely that more intensive blood pressure control improves cardiovascular outcomes and survival. 2 It also re-classified "pre-HTN" as elevated blood pressure (120-129/<80 mmHg). The last update was in 2017 and the major change at that time was lowering the definition of HTN from ≥140/≥90 mmHg to ≥130/≥80 mmHg. The AHA/ACC started synthesizing evidence and publishing guidelines specifically for HTN in 2014. 1 This is a welcome addition to the guidelines as it fills an important gap in the most recent AHA/American College of Cardiology (ACC) recommendations. The American Heart Association (AHA) has recently released a new Scientific Statement regarding management of stage 1 HTN in adults with a low 10-year risk for CVD. In recent years, the incidence and prevalence of HTN have increased while rates of HTN control have declined. More cardiovascular disease (CVD) events are attributable to hypertension (HTN) than any other modifiable CVD risk factor. If blood pressure remains uncontrolled at 3-6 months, consider starting pharmacologic therapy. Among low-risk adults (no ASCVD or 10-year CVD risk The AHA/ACC has released a scientific statement in 2021 offering new guidance for management of stage 1 hypertension among patients with low ASCVD risk.


 0 kommentar(er)
0 kommentar(er)
